- Home
-
SERVICES
Services offered by RM
-
SPECIALITIES
Major specialities
- WHY RM?
- SOFTWARES
- COMPLIANCES
- ABOUT US
Please fill out the form below if you have a plan or project in mind that you'd like to share with us.
Happy Clients
Projects Delivered
Skilled Employees
Support Available
A physician or other healthcare practitioner who want to treat patients who are members of a certain Payer's plans must first get credentialed, i.e., enrolled and attested with the Payer's network and approved to perform the Services in question. The Payer checks the doctor's credentials (such as their education, license, experience, certifications, affiliations, malpractice, adverse clinical events, and training) to ensure they are up to par before allowing them to treat patients.
Doctors who aren't credentialed and enrolled with a specific insurance company may have their payments held up or perhaps be denied entirely. The practice's bottom line suffers as a result of these factors. Doctors can rely on our individualized Payer certification and enrollment Services.
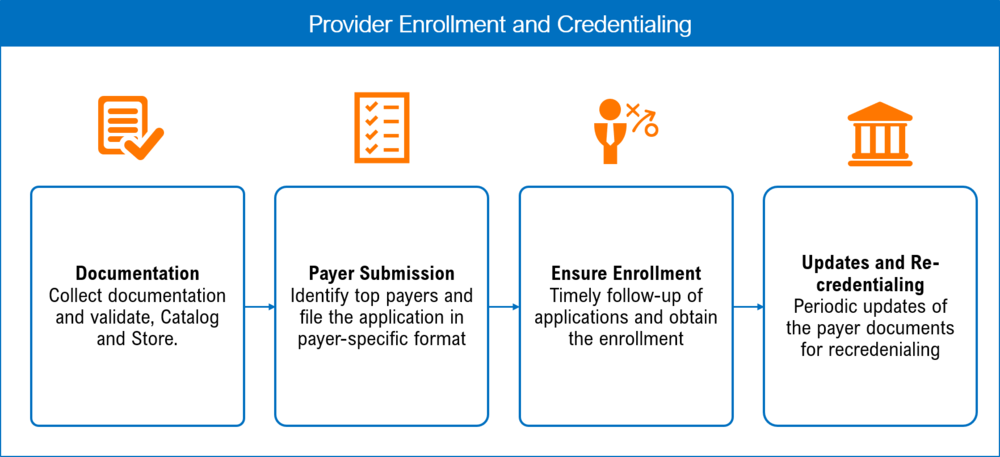
Our customized Payer credentialing and enrollment Services support physicians in :
Council for Affordable Quality Healthcare, Inc. eliminates redundant and inefficient administrative processes between health plans and providers for credentialing, directory maintenance, coordination of benefits, and other essential business functions.
With our diligent credentialing and Enrollment Services, you get the following benefits:
















