- Home
-
SERVICES
Services offered by RM
-
SPECIALITIES
Major specialities
- WHY RM?
- SOFTWARES
- COMPLIANCES
- ABOUT US
Please fill out the form below if you have a plan or project in mind that you'd like to share with us.
Happy Clients
Projects Delivered
Skilled Employees
Support Available
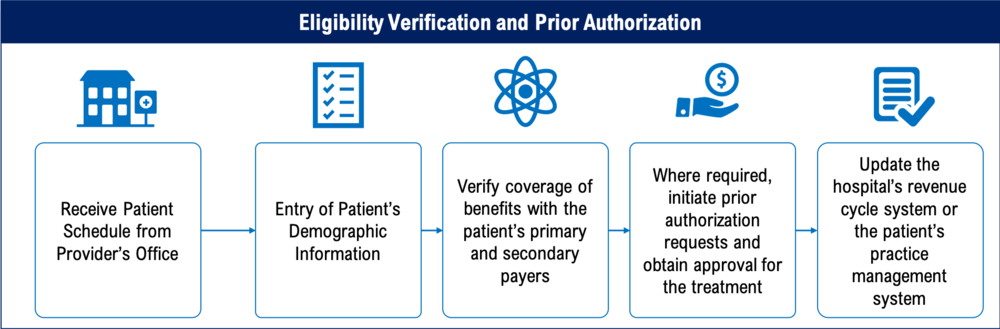
Verifying eligibility and insurance is critical for providing accurate coverage details in a timely manner. A healthcare provider may be leaving money on the table without adequate controls in place. A reduction in collections and revenues may occur from a failure to verify eligibility and obtain prior authorization.
Healthcare providers can better understand their patients' coverage, out-of-network benefits, and financial responsibility if eligibility is determined quickly and accurately up front. Eligibility verification procedures aid in the submission of accurate claims by healthcare providers. Claims are less likely to be rejected or denied based on patient demographics or insurance eligibility, and more money is collected up front, all of which contribute to happier patients and smoother medical billing processes. The Prior Authorization and Eligibility Verification Services provided by RM Healthcare will help you maximize your revenue cycle efficiency and increase your cash inflow.